Dummy
Torn meniscus
Information about the torn meniscus
General
Cause
Symptoms
Exam
Treatment
Age
What is a meniscus?
The knee joint consists of several bone pieces: the upper leg (femur), tibia (tibia) and kneecap (patella). The bones hinge smoothly with each other through a thick layer of cartilage. On top of the cartilage of the tibia are two menisci (meniscus). There is one meniscus on the inside (medial) and one on the outside (lateral).
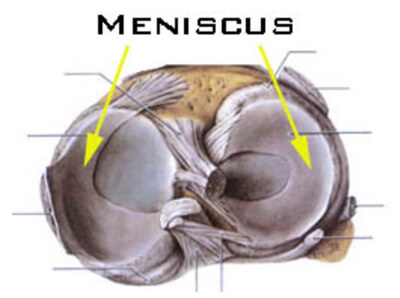
A meniscus is made up of cartilage (feel your earlobe to feel what cartilage is). The function of the meniscus is to protect the lower and upper cartilage and give stability to the knee joint.
Intacte meniscus
A torn meniscus can happen to anyone and at any age. Roughly speaking, two groups are distinguished. Persons younger, or older than 45 years of age. A torn meniscus in people under the age of 45 usually occurs due to a sports injury or a wrong movement in everyday life. The acting forces on the meniscus are great during sports and, unfortunately, things sometimes go wrong.
As one ages (>45 years), the quality of the meniscus decreases. Thus, the risk of a meniscus tear increases with age.
How does a meniscus tear occur?
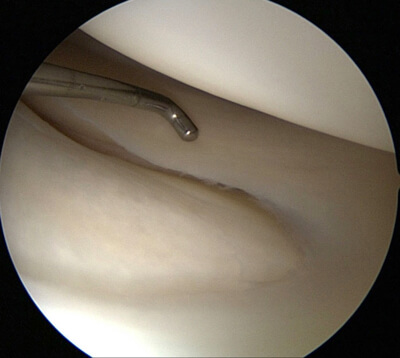
A torn meniscus is divided into two groups: an acute and degenerative meniscus tear. An acute torn meniscus is caused by excessive mechanical pressure on the knee during twisting, maximum flexion or overstretching. A bent knee with a twist is the most notorious movement for a meniscus tear.
Acute meniscus lesion
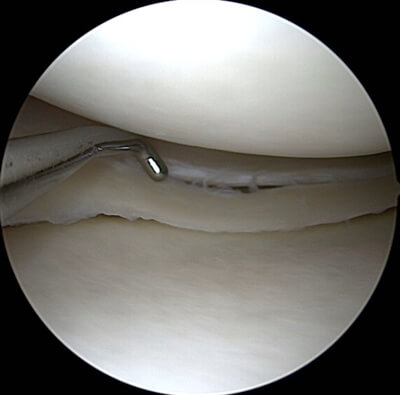
A degenerative meniscus tear occurs mainly in people 45 and older. The quality of the meniscus gradually deteriorates due to the natural aging process. The degeneration of the meniscus is accelerated by obesity, heavy physical work and intense sports. The characteristic of a degenerative meniscus, is that it has small hairline cracks and the meniscus is no longer evenly smooth. Because of the reduced quality, relatively high loads (jumping/running) or endurance loads (walking/yard work) are a cause of symptoms.
Degenerative meniscus lesion
Many people have abnormalities in their meniscus without having symptoms. If you take an MRI of a hundred random people over the age of 50, 35 percent will show a degenerative meniscus tear. And more often in men than women. As one gets older, the chance of a degenerative meniscus tear increases. The majority have no symptoms. An interesting question is why one person has symptoms with the same degenerative meniscus tear and another does not. Much research has been done on this in recent years. The degree of training seems to play a major role.
The meniscus should be loaded in a healthy manner. Dosed loading helps keep the quality of the meniscus optimal. Older people predominantly move and exercise less and are usually a few pounds overweight. This makes the knee vulnerable. Training and exercising the muscles has a positive effect according to the latest studies.
What are the symptoms and complaints of a torn meniscus?
A torn meniscus can be recognized by three characteristics. A trauma moment, hearing a tearing sound and swelling in the knee within twelve to twenty-four hours. A torn meniscus causes pain on the inside or outside of the knee. The pain may radiate to the back of the knee. The swelling present causes a stiff knee and possibly difficulty bending and stretching the knee. In addition, the knee may feel unstable or even locked. A locked knee is a knee that literally cannot bend and extend and is most characteristic of a torn meniscus.
In daily life, you are usually limited with squatting and twisting of the leg and sports. Usually the symptoms decrease over time, with targeted physical therapy being able to positively affect recovery.
A knee with a degenerative meniscus can be approached in two ways. The first is that the tears in the meniscus are already present. Because of the reduced load capacity, the knee becomes irritated more quickly with improper movement or overloading.
A second possibility is that the meniscus is more likely to be damaged by improper movement due to its deteriorated condition. The pain is usually on the inside or outside of the knee and sometimes radiates to the hollow of the knee, calf and hamstring region. The knee is usually swollen and stiff which makes bending and stretching difficult. The characteristic locking symptoms are less common in degenerative meniscal lesions. In daily life, squatting, climbing stairs, walking, turning in bed and sleeping on the side can provoke pain.
How can you examine if your meniscus is torn?
Acute meniscus injury:
A meniscus lesion has a typical presentation of symptoms and can therefore be diagnosed fairly easily by the general practitioner. In an acute knee injury, however, multiple structures may be damaged. Making a diagnosis is more difficult, but an experienced physical therapist can make a good assessment of the injury based on the story and physical examination.
If the pain symptoms do not diminish with targeted physical therapy and/or treatment from the general practitioner, an orthopedic consultation may be considered. If a serious knee injury is suspected, a consultation with the orthopedist is advisable.
The orthopedist asks a number of questions and conducts physical examination. Should further examination be indicated, the MRI is the logical choice. A meniscus injury can be well mapped by the MRI. Seeing is believing, but an MRI is actually done only when the orthopedist suspects an operation indication. An MRI is a costly and time-intensive examination.
Degenerative meniscus injury:
A degenerative meniscus tear has broadly the same symptoms as an acute meniscus injury. The general practitioner and physical therapist can make a reasonable to good diagnosis through pointed questions and physical examination.
When there is a degenerative meniscus, there is usually some degree of wear and tear as well. An X-ray will provide more insight into this. There is usually no indication for an MRI. The reason is that the degree of wear and tear says nothing about the amount of complaints. In addition, based on the intake and examination, the cause of the pain can already be determined and an MRI is not necessary to confirm that.
Therefore, a referral to the orthopedist is not necessary. If you get stuck in the conservative course, a consultation may be considered.
What can you do about a torn meniscus?
In recent years, much research has been done on the treatment of a meniscus injury. In the past, a meniscus was removed without mercy, which greatly increased the risk of wear and tear Because of this, there has been a spike in people with wear and tear. The meniscus has an important function and that is to protect the underlying cartilage. Removing a piece of meniscus increases the pressure exceptionally. This also increases the chance of premature wear and tear. With today's knowledge, treatment has changed and is significantly more conservative. For both an acute and degenerative meniscus tear, exercise, training and physical therapy is the first choice.
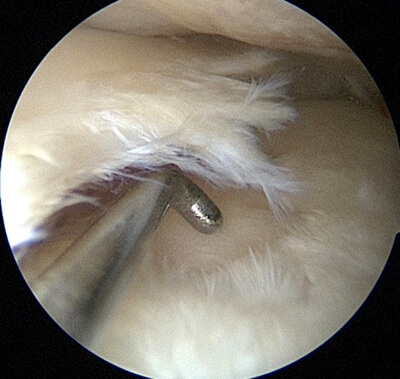
A locked knee due to a bucket handle (meaning the meniscus has been knocked over), for example, does indicate prompt surgery. Individually, it always remains important to weigh which treatment is the best fit.

Bucket handle meniscus
Rehabilitation for an acute meniscus injury initially focuses on reducing swelling and building muscle strength. Here it is important not to overstimulate the meniscus mechanically (maximum bending) and avoid rotations.
Note: swelling in the knee always results in decreased tension and control of the upper leg muscles.
Once the knee has come to rest, the muscles around the knee can begin to be strengthened. Here it is important to strengthen the entire chain.
If the load capacity of the knee and body increases, then the focus can be placed on sports-specific rehabilitation. If you get stuck in any of these phases, the first step is to evaluate and adjust the rehabilitation program. The main goal remains preserving the meniscus for as long as possible. If the knee remains unsettled with swelling, pain and movement restriction, it may be a consideration to adjust your goal. The alternative is a referral to the orthopedist to discuss surgery options.
The two options are a meniscectomy (remove piece of meniscus) and a meniscopexy (meniscus suture).
Often knee problems in degenerative meniscus arise from overuse. Underlying this are: insufficient training of the muscles, stability and coordination.
Treatment focuses on reducing swelling (if any), exercising the muscles, improving stability and coordination. Again, it is important to train the chain of the body. The first positive effects of treatment are experienced on average after six to eight weeks.
In consultation with your physician or physical therapist, you can weigh whether full sports resumption is possible again. After all, a degenerative meniscus tear often goes hand in hand with a certain degree of wear and tear that makes higher peak load and rotational movements permanently provocative.
A keyhole surgery in which the meniscus is trimmed generally has the same effect as long-term training.
Meniscus treatment by age
Younger than 45 years with acute meniscus pain
A healthy meniscus can tear due to a high impacting force. In most cases, it is wise to give the body a chance to heal (physical therapy, exercises, adjusting load). If it is a small tear in the perfused part of the meniscus, it can repair itself (partially). The pain and limitations in daily life decrease and sports resumption is possible again. Take your time (about 6 weeks) and be patient. Remember that it is especially beneficial in the long term for the knee not to have surgery.
If the knee does not recover sufficiently, it is wise to have an MRI scan to accurately assess the meniscus. Depending on the findings, surgery may be considered. If the meniscus is large or folded over (bucket handle) and the knee is locked, then surgery will be performed with some urgency.
During surgery, an assessment will be made as to whether the meniscus can be sutured or partially cut. The preferred option is to suture the meniscus. This preserves the function of the meniscus. Less favorable in the long term is to (partially) cut away the meniscus. It increases the risk of osteoarthritis.
Younger than 45 years degenerative meniscus complaints
When the quality of the meniscus diminishes, it can cause knee problems. In the past, these complaints used to require surgery. Today, the recommendation is 6 to 12 weeks of conservative rehabilitation. Recovery focuses on improving muscle strength, stability, coordination, load management and advice to avoid provocative actions. The physical therapist can be very helpful in this regard.
If the knee does not recover sufficiently, an orthopedist may be consulted after 6 to 12 weeks. If there are minimal to no abnormalities on the radiograph, an MRI may be considered. Before this is done, physical therapy is critically examined. If necessary, another referral to a specialized knee physical therapist for targeted exercises can be made through the orthopedist's network. Suturing a meniscus is not possible due to its reduced quality. Removing a piece of the meniscus is possible and can reduce the symptoms. But research shows that the difference with a conservative policy is almost negligible. In the process, you lose part of your shock absorber, increasing the risk of osteoarthritis. For this reason, conservative treatment is preferred.
Over 45 years of age with acute or degenerative meniscus pain
Meniscus complaints that arise over the age of 45 are almost always caused by a degenerative meniscus. Even with acute injury, there is almost always degenerative meniscus tear. The treatment instituted is actually always conservative. Take your time and be patient. On average, you need 8 to 12 weeks to notice good effects from conservative treatment. Surgery is not recommended, because recent research shows that in the longer term the effect is almost the same as the conservative course.
Meniscus injury i.c.w. accompanying injuries (e.g., torn anterior cruciate ligament)
Meniscus injury can be accompanied by damage to other structures in the knee. For example, tearing of the VKB is often accompanied by meniscus injury. For proper repair of the meniscus, the knee must be stable. Therefore, when a meniscus suture is made, the VKB is also repaired at the same time or soon in a second operation.
Meniscus injury in elite athletes
In elite sports, there is always time pressure and surgical intervention is generally chosen quickly. Often top athletes are still young, which makes suturing the meniscus possible. This is positive for the longer term, but in the short term, rehabilitation takes longer and there is a chance that the suture will fail. In that case, the meniscus will still have to be cut and the entire rehabilitation will take longer. After taking the MRI to confirm the diagnosis, part of the meniscus is removed during surgery. This is generally followed by short-term rehabilitation.
