Dummy
Cartilage damage cause symptoms and treatment
Information about cartilage damage
When faced with cartilage damage, you will undoubtedly be left with questions. Probably the most important question is what treatment for a cartilage injury looks like. Is surgery necessary, or can the knee recover without surgery (conservatief). Om deze vragen te beantwoorden, is het essentieel om eerst te begrijpen wat kraakbeenschade precies is en verkennen we de oorzaken, symptomen en behandeling. Hier lees je alles over kraakbeenschade.
General
Cause
Symptoms
Exam
Treatment
What is cartilage
Knee cartilage is an essential part of the knee joint that allows the knee to move smoothly. Cartilage is a tough, elastic tissue that covers the ends of bones. Because of its specialized properties, cartilage acts as a shock absorber. Unfortunately, knee cartilage is susceptible to wear and damage, which can lead to conditions such as cartilage defects and eventually knee osteoarthritis.
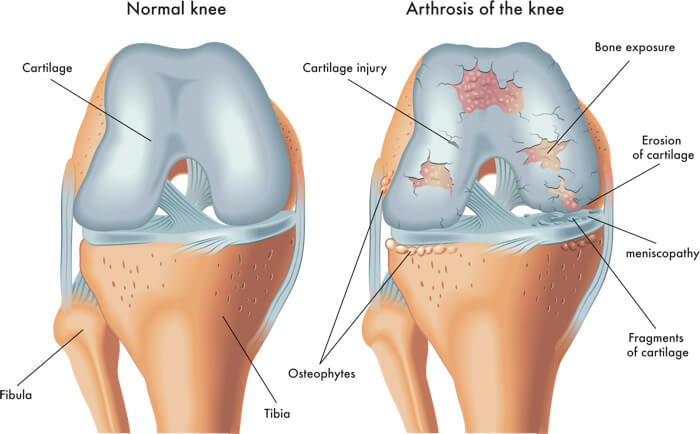
Various forms of cartilage damage.
What is cartilage damage?
Cartilage damage means that there is damage present in the cartilage layer. It is similar to a hole in the enamel a tooth. The location of the cartilage damage varies, but is usually related to the impact of the knee injury or peak loading due to certain sports and/or anatomy of the knee. Cartilage damage is about the width of the injury on the one hand but also about the depth. To grade depth, there is a scale to indicate severity.
The grades for cartilage damage:
Grade 0: no cartilage damage
Grade 1: superficial lesions
Grade 2: cartilage damage up to 50% depth
Grade 3: deeper than 50%
Grade 4: to the underlying bone.
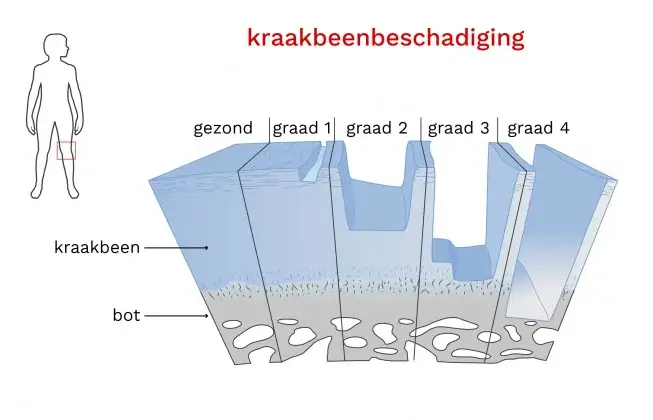
gradaties kraakbeenschade
What are causes of cartilage damage?
Cartilage damage in the knee has several causes. The most obvious is a knee injury, such as a sports injury or an accident where the knee undergoes impact or twisting. Cartilage can handle pressure well, but pressure combined with a rotational component is more difficult. An anterior cruciate ligament injury is typically a knee injury in which both components take place. In addition, there is (sub)luxation of the lower leg relative to the upper leg, causing both bone pieces to collide. This is one reason for the commonly occurring bone bruising and poses a risk for cartilage damage (see video). The same can happen with (sub)luxation of the kneecap. The luxation causes the kneecap to collide with the side of the kneecap's gutter, and there is also a collision between the kneecap and the edge of the gutter as it goes back into the gutter.
A knee injury is a risk factor for cartilage damage. If there is a ligament injury, the risk increases, but even more so if there is also a meniscus injury. Until not so long ago, a torn meniscus was removed or a piece of it cut away. However, the pressure on the cartilage then increases by 80-90%, so today we opt for suturing or waiting without surgery. "Save the meniscus" is a common cry at conferences.
Another cause of cartilage damage is excessive stress or repeated stress on the knee. Here we speak of microtraumas, which occur in various sports (soccer, gymnastics, basketball, volleyball, etc.) and occupations. The repetitive microtraumas can cause cartilage damage. Furthermore, degenerative conditions such as osteoarthritis are major causes of cartilage damage. Risk factors for this include an x- or o-leg axis, which may or may not be combined with obesity. If you want to learn more about osteoarthritis, click here.
What are the symptoms and complaints after cartilage damage?
The most recognizable symptom and complaint with cartilage damage is pain. The pain is usually located on the inside, outside and/or front of the knee. In addition to pain, the knee may feel stiff and swollen to a greater or lesser degree after loading. Swelling is a sign of irritation or overuse of the knee. Due to the pain, sports are no longer always possible or the load must be adjusted. For example, you can think about running 5 kilometers instead of 10 kilometers, playing half a soccer game instead of a full one, or cycling and swimming more instead of playing tennis. Another option is playing doubles tennis instead of singles.
How do you examine a knee with cartilage damage?
Examining a knee with suspected cartilage injury is difficult. This is because the symptoms closely resemble meniscus-related symptoms or patellofemoral pain syndrome, should the pain be felt at the front of the knee. Physical examination can fairly well assess whether it is a knee problem in the joint or outside the joint, as is the case with a tendon complaint, for example. Physical examination usually includes checking range of motion, stability and the presence of swelling in the knee.
With an acute knee injury, an MRI scan is usually performed, which quickly reveals whether cartilage damage (also) exists. It can also happen that the symptoms have developed gradually. An MRI scan is then often made at a later stage. For the treatment of cartilage defects, it does not matter whether it is diagnosed early or late. An X-ray is routinely done at the orthopedic surgeon's office. You won't see cartilage on these photos, but you may see bone abnormalities that are indicative of cartilage quality.
In some cases, arthroscopy, a surgical procedure in which a small camera is inserted into the knee, can be performed to obtain a direct view of the cartilage. This allows doctors to more accurately assess the injury and, if necessary, perform minor surgery to treat the cartilage at the same time.
What does treatment look like for cartilage damage?
Treatment of cartilage damage in the knee depends on several factors, including the extent of the injury, its location and the patient's overall health. In some cases, conservative treatment may be sufficient, while others require more specialized interventions.
Conservative treatments often include rest, physical therapy and medication for pain relief and anti-inflammation. Physical therapy focuses on strengthening the muscles around the knee, promoting stability and improving mobility. If excess weight is present, weight management may be recommended to reduce stress on the knee joint.
More severe cartilage damage may require surgical intervention. A common procedure is arthroscopy, in which small incisions are made and a camera is inserted to evaluate and, if possible, repair the damaged cartilage. In some cases, microfracture technique may be used to stimulate the formation of new cartilage.
For more extensive cartilage damage, autologous cartilage transplantation or allogeneic cartilage cell transplantation may be considered. This involves transplanting healthy cartilage tissue from elsewhere in the body (autologous) or from a donor (allogeneic) into the damaged area of the knee.
Recent developments also include regenerative drugs, such as stem cell therapy and growth factors, which aim to stimulate the cartilage's natural healing processes.
Each treatment option has its own advantages and disadvantages, and the choice depends on the specifics of the injury and the patient's individual circumstances. A thorough evaluation by a specialized health care provider is essential to establish an appropriate treatment plan for knee cartilage injuries.
In summary, the following treatment options are the most commonly used in the Netherlands:
- Conservative treatment with or without physical therapy
- Operatie middels microfactuurtechniek
- Autologe kraakbeenceltransplantatie (ACI)
- Matrix-assisted autologous cartilage cell transplantation(MACT)
- Osteochondral autograft transplantation (OATS)
This text is supplemented by blogs.
